Overview
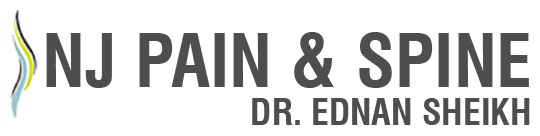
Spinal cord stimulation (also called SCS) uses electrical impulses to relieve chronic pain of the back, arms and legs. It is believed that electrical pulses prevent pain signals from being received by the brain. SCS candidates include people who suffer from neuropathic pain and for whom conservative treatments have failed.
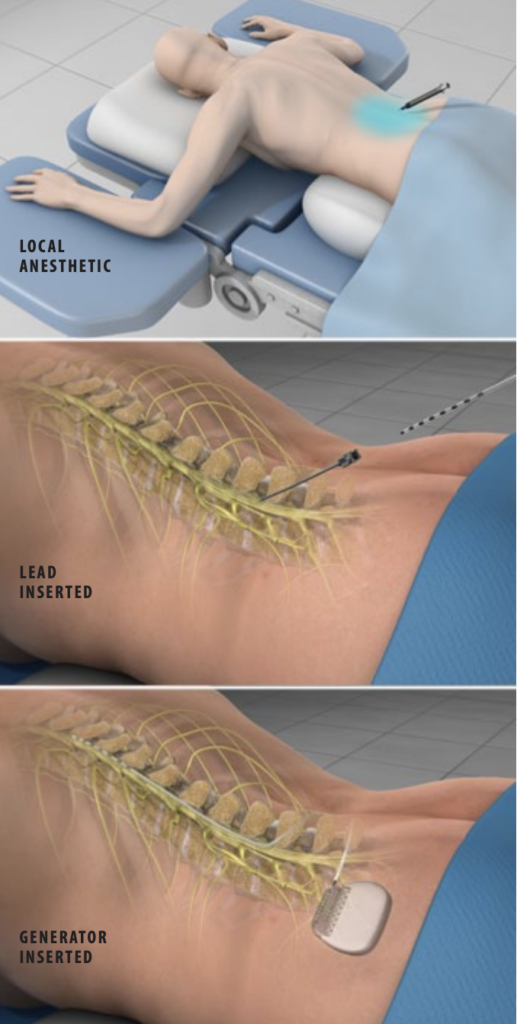
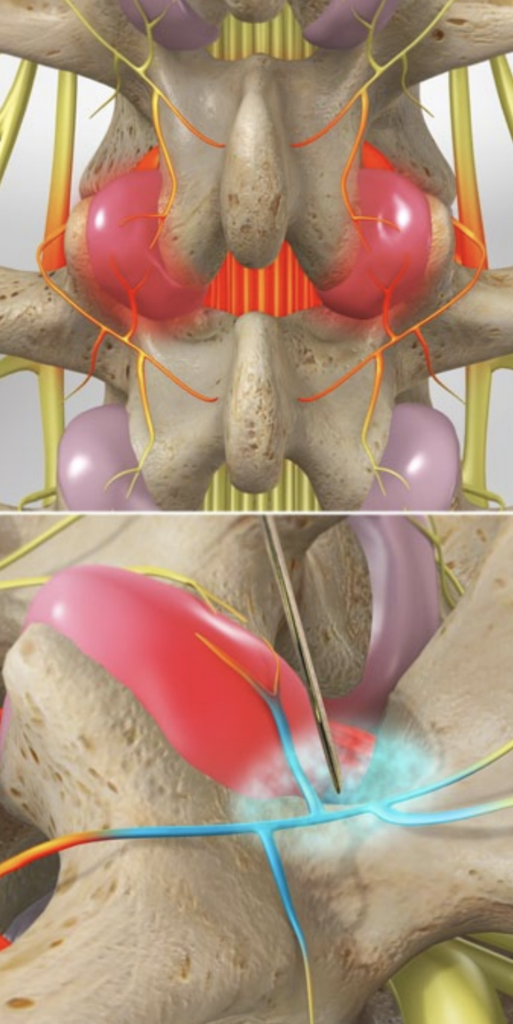
Trial Implantation
The injection site is anesthetized. One or more insulated wire leads are inserted through an epidural needle or through a small incision into the space surrounding the spinal cord, called the epidural space.
Find the Right Location
Electrodes at the end of the lead produce electrical pulses that stimulate the nerves, blocking pain signals. The patient gives feedback to help the physician determine where to place the stimulators to best block the patient’s pain. The leads are connected to an external trial stimulator, which will be used for approximately one week to determine if SCS will help the patient.
Determine Effectiveness
If the patient and the physician determine that the amount of pain relief is acceptable, the system may be permanently implanted. At the end of the trial implantation, the leads are removed.
Permanent Implantation
The permanent implantation may be performed while the patient is under sedation or general anesthesia. First, one or more permanent leads are inserted through an epidural needle or a small incision into the predetermined location in the epidural space.
Generator Implantation
Next, a small incision is created, and the implantable pulse generator (IPG) battery is positioned beneath the skin. It is most often implanted in the buttocks or the abdomen. The leads are then connected to the IPG battery.
End of Procedure
The implant’s electrical pulses are programmed with an external wireless programmer. The patient can use the programmer to turn the system on or off, adjust the stimulation power level and switch between different programs.
After SCS Implantation
After surgery, patients may experience mild discomfort and swelling at the incision sites for several days.
 Overview
Overview